REZUROCK was evaluated in the pivotal ROCKstar (KD025-213) study in a real-world demographic of patients with cGVHD1,2
The FDA approval of REZUROCK was based on the pivotal ROCKstar study.1
The ROCKstar study included a broad range of patients who were representative of the general cGVHD population.1,2
These patients had
- Early-stage cGVHD as well as late-stage disease1,2
- Diverse ages (≥12 years)1
- NIH-defined moderate (27%) or severe (70%) cGVHD2
- A wide range of organ involvement, including fibrotic manifestations1,2
- A diverse treatment history1,2
- Median of 3 prior lines of systemic therapy (30% had received ruxolitinib and 33% had received ibrutinib)2
.png 375w)
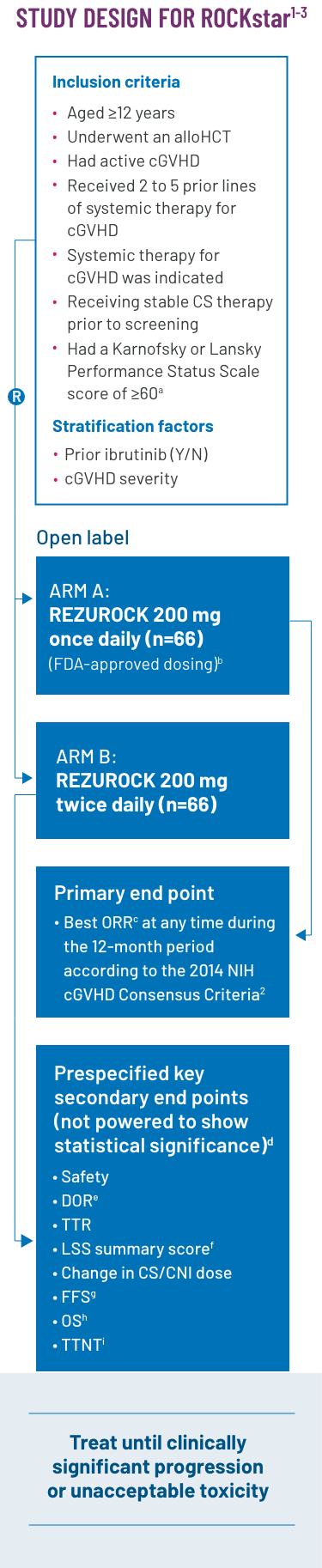
ROCKstar was a pivotal phase 2, open-label, randomized, multicenter study that evaluated the efficacy and safety of REZUROCK in patients with cGVHD after receiving 2 to 5 prior lines of systemic therapy.1,2
Exclusion criteria: Patients were excluded from the study if they had a relapse of their underlying malignancy, had developed posttransplant lymphoproliferative disease, were currently receiving ibrutinib2 or had any of the following laboratory results: platelets were <50 × 109/L; absolute neutrophil count <1.5 × 109/L; AST or ALT >3 × ULN; total bilirubin >1.5 × ULN; QTc(F) >480 ms; eGFR <30 mL/min/1.73 m2; or FEV1 ≤39%.1
aThe Karnofsky/Lansky Performance Status Scale is used in outcome-based analyses to determine the functional status of a patient. The Karnofsky Scale is designed for patients aged ≥16 years, whereas the Lansky Scale is designed for patients aged <16 years. The scale range for both is 10 to 100.4
bThe final FDA interpretation of the ROCKstar study omitted 1 patient from the REZUROCK 200-mg once-daily arm. As a result, there are minor differences between the ROCKstar publication, where n=66, and the Prescribing Information, where n=65.
cORR was defined as the proportion of patients who achieved CR or PR according to the 2014 NIH cGVHD Consensus Criteria.1,2
dPrespecified secondary end points; not powered to show statistical significance.
eDOR was measured from the time of initial PR or CR until documented progression from best response of cGVHD, time from initial response to start of additional systemic cGVHD therapy or death.2
fThe 7-day LSS summary score was calculated based on the developer recommendations and was compared with the score from baseline in an exploratory analysis. An improvement of ≥7 points was considered clinically meaningful.2
gFFS was defined as the absence of relapse, nonrelapse mortality or a need for additional systemic therapy.2
hOS was defined as the time from the first dose of REZUROCK to the date of death due to any cause.3
iTTNT was defined as the time from the first dose of REZUROCK to the start of additional systemic cGVHD therapy.3
Screening for eligibility was conducted within 14 days of C1D1.2
Certain concurrent immunosuppressive medications were allowed, as drug-drug interactions were not anticipated.2
SELECT BASELINE CHARACTERISTICS2,3
The baseline demographics demonstrate the diversity of the patient population in the ROCKstar study. Many patients presented with challenging characteristics, including advanced or complex disease and having received multiple prior lines of systemic therapy.
| Characteristics | REZUROCK 200 mg once daily (n=66)b |
|---|---|
| Median age, y (range) | 53 (21-77) |
| Male, n (%) | 42 (64) |
| Median prior lines of systemic therapy, n | 3 |
| Median time from cGVHD diagnosis to enrollment, mo (range) | 25 (2-162) |
| Median prednisone-equivalent dose at enrollment, mg/kg/d (range) | 0.20 (0.03-0.95) |
| Concomitant PPI use, n (%) | 33 (50) |
| ≥4 organs involved, n (%) | 33 (50) |
| Previous aGVHD, n (%) | 42 (64) |
| Refractory to prior line of systemic therapy, n (%) | 44 (79j) |
| NIH-defined cGVHD severity, n (%) | |
| Severe | 46 (70) |
| Moderate | 18 (27) |
| Mild | 2 (3) |
| Prior systemic cGVHD therapy type, n (%) | |
| CS (prednisone) | 65 (99) |
| Tacrolimus | 40 (61) |
| ECP | 31 (47) |
| Sirolimus | 29 (44) |
| Ibrutinib | 22 (33) |
| Ruxolitinib | 20 (30) |
| Cyclosporine | 4 (6) |
| Imatinib | 3 (5) |
bThe final FDA interpretation of the ROCKstar study omitted 1 patient from the REZUROCK 200-mg once-daily arm. As a result, there are minor differences between the ROCKstar publication, where n=66, and the Prescribing Information, where n=65.
jDenominator excludes patients with unknown status.1
MOST PATIENTS IN THE ROCKstar STUDY HAD MODERATE OR SEVERE cGVHD
BASED ON THE 2014 NIH cGVHD CONSENSUS CRITERIA2

bThe final FDA interpretation of the ROCKstar study omitted 1 patient from the REZUROCK 200-mg once-daily arm. As a result, there are minor differences between the ROCKstar publication, where n=66, and the Prescribing Information, where n=65.
A BROAD RANGE OF
ORGAN INVOLVEMENT2
| Organ involvement |
Patients (n=66),b |
|---|---|
| Eyes | 48 (73) |
| Skin | 55 (83) |
| Mouth | 30 (46) |
| Joints/Fascia | 51 (77) |
| Lungs | 24 (36) |
| Upper GI | 13 (20) |
| Esophagus | 19 (29) |
| Lower GI | 6 (9) |
| Liver | 9 (14) |
bThe final FDA interpretation of the ROCKstar study omitted 1 patient from the REZUROCK 200-mg once-daily arm. As a result, there are minor differences between the ROCKstar publication, where n=66, and the Prescribing Information, where n=65.
EFFICACY WAS ACHIEVED
in a real-world demographic of patients.1,2,k
aGVHD, acute graft-versus-host disease; alloHCT, allogeneic hematopoietic cell transplant; ALT, alanine aminotransferase; AST, aspartate aminotransferase; cGVHD, chronic graft-versus-host disease; C1D1, cycle 1 day 1; CNI, calcineurin inhibitor; CR, complete response; CS, corticosteroid(s); DOR, duration of response; ECP, extracorporeal photopheresis; eGFR, estimated glomerular filtration rate; FDA, US Food and Drug Administration; FEV1, forced expiratory volume in 1 second; FFS, failure-free survival; GI, gastrointestinal; LSS, Lee Symptom Scale; MOA, mechanism of action; NIH, National Institutes of Health; ORR, overall response rate; OS, overall survival; PPI, proton pump inhibitor; PR, partial response; TTNT, time to next treatment; TTR, time to response; ULN, upper limit of normal.
jDenominator excludes patients with unknown status.1
kROCKstar study select baseline patient characteristics (200-mg once-daily arm): Median age of 53 years (range, 21-77); male, n=42 (64%); median of 3 prior lines of systemic therapy; median of 25 months (range, 2-162) from cGVHD diagnosis to enrollment; median prednisone-equivalent dose at enrollment of 0.20 mg/kg/d (range, 0.03-0.95); concomitant PPI use, n=33 (50%); ≥4 organs involved, n=33 (50%); previous aGVHD, n=42 (64%); refractory to prior line of systemic therapy, n=44 (79%j); NIH-defined disease severity: n=46 (70%) severe, n=18 (27%) moderate, n=2 (3%) mild. Prior systemic therapies included corticosteroids (prednisone), n=65 (99%); tacrolimus, n=40 (61%); ECP, n=31 (47%); ibrutinib, n=22 (33%); and ruxolitinib, n=20 (30%).2,3
References: 1. REZUROCK. Package insert. Kadmon Pharmaceuticals, LLC. 2. Cutler C, Lee SJ, Arai S, et al; on behalf of the ROCKstar Study Investigators. Belumosudil for chronic graft-versus-host disease after 2 or more prior lines of therapy: the ROCKstar Study. Blood. 2021;138(22):2278-2289. doi:10.1182/blood.2021012021 3. Data on file. Sanofi. 4. Center for International Blood and Marrow Transplant Research. Karnofsky/Lansky performance status. Accessed March 24, 2025. https://cibmtr.org/Files/Data-Operations/Retired-Forms-Manuals/Appendices/appendix-l.pdf
INDICATION
IMPORTANT SAFETY INFORMATION
IMPORTANT SAFETY INFORMATION
INDICATION
REZUROCK® (belumosudil) is indicated for the treatment of adult and pediatric patients 12 years and older with chronic graft-versus-host disease (chronic GVHD) after failure of at least two prior lines of systemic therapy.
IMPORTANT SAFETY INFORMATION
Warnings and Precautions
- Embryo-Fetal Toxicity: Based on findings in animals and its mechanism of action, REZUROCK can cause fetal harm when administered to a pregnant woman. Advise pregnant women of the potential risk to a fetus. Advise females of reproductive potential and males with female partners of reproductive potential to use effective contraception during treatment with REZUROCK and for one week after the last dose
Adverse Reactions
- The most common (≥ 20%) adverse reactions, including laboratory abnormalities, were infections, asthenia, nausea, diarrhea, dyspnea, cough, edema, hemorrhage, abdominal pain, musculoskeletal pain, headache, phosphate decreased, gamma glutamyl transferase increased, lymphocytes decreased, and hypertension
- Permanent discontinuation of REZUROCK due to adverse reactions occurred in 18% of patients. The adverse reactions which resulted in permanent discontinuation of REZUROCK in > 3% of patients included nausea (4%). Adverse reactions leading to dose interruption occurred in 29% of patients. The adverse reactions leading to dose interruption in ≥ 2% were infections (11%), diarrhea (4%), and asthenia, dyspnea, hemorrhage, hypotension, liver function test abnormal, nausea, pyrexia, edema, and renal failure with (2% each)
- Monitor total bilirubin, aspartate aminotransferase (AST), and alanine aminotransferase (ALT) at least monthly
Drug Interactions
- Proton Pump Inhibitors: Belumosudil exhibits pH-dependent solubility. Concomitant use of REZUROCK with proton pump inhibitors decreases belumosudil exposure, which may reduce the efficacy of REZUROCK. Increase the dosage of REZUROCK when used concomitantly with proton pump inhibitors
- Strong CYP3A Inducers: Belumosudil is a CYP3A substrate. Concomitant use of REZUROCK with strong CYP3A inducers decreases belumosudil exposure which may reduce the efficacy of REZUROCK. Increase the dosage of REZUROCK when used concomitantly with strong CYP3A inducers
- BCRP and OATP1B1 Substrates: Avoid concomitant use with drugs that are BCRP substrates where possible. If used together, monitor patients more frequently for adverse reactions and decrease the BCRP substrates dosage(s) in accordance with the respective Prescribing Information.
Belumosudil is a BCRP inhibitor. Concomitant use of REZUROCK with BCRP substrates increases their plasma concentrations, which may increase the risk of adverse reactions related to these substrates.
Belumosudil is an OATP1B1 inhibitor. Concomitant use of REZUROCK with OATP1B1 substrates may increase their plasma concentrations. Monitor patients more frequently for adverse reactions of these substrates and decrease the OATP1B1 substrates dosage(s) in accordance with the respective Prescribing Information - Certain CYP1A2 and CYP3A Substrates: Avoid concomitant use of REZUROCK with drugs that are sensitive CYP1A2 or CYP3A substrates, for which minimal concentration changes may lead to serious toxicities. If concomitant use cannot be avoided, decrease the CYP1A2 or CYP3A substrate dosage(s) in accordance with the respective Prescribing Information. Belumosudil is a CYP1A2 and CYP3A inhibitor. Concomitant use of REZUROCK with sensitive CYP1A2 substrates (e.g., caffeine) or CYP3A substrates (e.g., midazolam) is predicted to increase CYP1A2 or CYP3A substrate exposure, which may increase the risk of adverse reactions related to these substrates
- Certain UGT1A1 Substrates: Avoid concomitant use of REZUROCK with drugs that are UGT1A1 substrates, for which minimal concentration changes may lead to serious toxicities. If concomitant use cannot be avoided, decrease the UGT1A1 substrates dosage(s) in accordance with the respective Prescribing Information. Belumosudil is a UGT1A1 inhibitor. Concomitant use of REZUROCK with a UGT1A1 substrate decreased plasma concentrations of the glucuronide metabolite of the UGT1A1 substrate. Concomitant use of belumosudil with other UGT1A1 substrates may increase their plasma concentrations, which may increase the risk of adverse reactions related to these substrates
- Certain P-gp Substrates: Avoid concomitant use of REZUROCK with drugs that are P-gp substrates, for which minimal concentration changes may lead to serious toxicities. If concomitant use cannot be avoided, decrease the P-gp substrates dosage(s) in accordance with the respective Prescribing Information. Belumosudil is a P-gp inhibitor. Concomitant use of REZUROCK with P-gp substrates increased their plasma concentrations, which may increase the risk of adverse reactions related to these substrates
Use in Specific Populations
- Pregnancy: There are no available human data on REZUROCK use in pregnant women to evaluate for a drug-associated risk. Advise pregnant women and females of reproductive potential of the potential risk to the fetus
- Lactation: There are no data available on the presence of belumosudil or its metabolites in human milk or the effects on the breastfed child, or milk production. Because of the potential for serious adverse reactions from belumosudil in the breastfed child, advise lactating women not to breastfeed during treatment with REZUROCK and for one week after the last dose
- Pediatric Use: The safety and effectiveness of REZUROCK in pediatric patients less than 12 years old have not been established
- Geriatric Use: Of the 186 patients with chronic GVHD in clinical studies of REZUROCK, 26% were 65 years and older. No clinically meaningful differences in safety or effectiveness of REZUROCK were observed in comparison to younger patients
- Renal Impairment: Treatment with REZUROCK has not been studied in patients with pre-existing severe renal impairment. For patients with pre-existing severe renal impairment, consider the risks and potential benefits before initiating treatment with REZUROCK
- Hepatic Impairment: Avoid use in patients with moderate hepatic impairment (Child-Pugh B) or severe hepatic impairment (Child-Pugh C) without liver GVHD. No dose adjustment is recommended for patients with mild hepatic impairment (Child-Pugh A)
Please click here for full Prescribing Information.
IMPORTANT SAFETY INFORMATION
Warnings and Precautions
- Embryo-Fetal Toxicity: Based on findings in animals and its mechanism of action, REZUROCK can cause fetal harm when administered to a pregnant woman. Advise pregnant women of the potential risk to a fetus. Advise females of reproductive potential and males with female partners of reproductive potential to use effective contraception during treatment with REZUROCK and for one week after the last dose
Adverse Reactions
- The most common (≥ 20%) adverse reactions, including laboratory abnormalities, were infections, asthenia, nausea, diarrhea, dyspnea, cough, edema, hemorrhage, abdominal pain, musculoskeletal pain, headache, phosphate decreased, gamma glutamyl transferase increased, lymphocytes decreased, and hypertension
- Permanent discontinuation of REZUROCK due to adverse reactions occurred in 18% of patients. The adverse reactions which resulted in permanent discontinuation of REZUROCK in > 3% of patients included nausea (4%). Adverse reactions leading to dose interruption occurred in 29% of patients. The adverse reactions leading to dose interruption in ≥ 2% were infections (11%), diarrhea (4%), and asthenia, dyspnea, hemorrhage, hypotension, liver function test abnormal, nausea, pyrexia, edema, and renal failure with (2% each)
- Monitor total bilirubin, aspartate aminotransferase (AST), and alanine aminotransferase (ALT) at least monthly
Drug Interactions
- Proton Pump Inhibitors: Belumosudil exhibits pH-dependent solubility. Concomitant use of REZUROCK with proton pump inhibitors decreases belumosudil exposure, which may reduce the efficacy of REZUROCK. Increase the dosage of REZUROCK when used concomitantly with proton pump inhibitors
- Strong CYP3A Inducers: Belumosudil is a CYP3A substrate. Concomitant use of REZUROCK with strong CYP3A inducers decreases belumosudil exposure which may reduce the efficacy of REZUROCK. Increase the dosage of REZUROCK when used concomitantly with strong CYP3A inducers
- BCRP and OATP1B1 Substrates: Avoid concomitant use with drugs that are BCRP substrates where possible. If used together, monitor patients more frequently for adverse reactions and decrease the BCRP substrates dosage(s) in accordance with the respective Prescribing Information.
Belumosudil is a BCRP inhibitor. Concomitant use of REZUROCK with BCRP substrates increases their plasma concentrations, which may increase the risk of adverse reactions related to these substrates.
Belumosudil is an OATP1B1 inhibitor. Concomitant use of REZUROCK with OATP1B1 substrates may increase their plasma concentrations. Monitor patients more frequently for adverse reactions of these substrates and decrease the OATP1B1 substrates dosage(s) in accordance with the respective Prescribing Information - Certain CYP1A2 and CYP3A Substrates: Avoid concomitant use of REZUROCK with drugs that are sensitive CYP1A2 or CYP3A substrates, for which minimal concentration changes may lead to serious toxicities. If concomitant use cannot be avoided, decrease the CYP1A2 or CYP3A substrate dosage(s) in accordance with the respective Prescribing Information. Belumosudil is a CYP1A2 and CYP3A inhibitor. Concomitant use of REZUROCK with sensitive CYP1A2 substrates (e.g., caffeine) or CYP3A substrates (e.g., midazolam) is predicted to increase CYP1A2 or CYP3A substrate exposure, which may increase the risk of adverse reactions related to these substrates
- Certain UGT1A1 Substrates: Avoid concomitant use of REZUROCK with drugs that are UGT1A1 substrates, for which minimal concentration changes may lead to serious toxicities. If concomitant use cannot be avoided, decrease the UGT1A1 substrates dosage(s) in accordance with the respective Prescribing Information. Belumosudil is a UGT1A1 inhibitor. Concomitant use of REZUROCK with a UGT1A1 substrate decreased plasma concentrations of the glucuronide metabolite of the UGT1A1 substrate. Concomitant use of belumosudil with other UGT1A1 substrates may increase their plasma concentrations, which may increase the risk of adverse reactions related to these substrates
- Certain P-gp Substrates: Avoid concomitant use of REZUROCK with drugs that are P-gp substrates, for which minimal concentration changes may lead to serious toxicities. If concomitant use cannot be avoided, decrease the P-gp substrates dosage(s) in accordance with the respective Prescribing Information. Belumosudil is a P-gp inhibitor. Concomitant use of REZUROCK with P-gp substrates increased their plasma concentrations, which may increase the risk of adverse reactions related to these substrates
Use in Specific Populations
- Pregnancy: There are no available human data on REZUROCK use in pregnant women to evaluate for a drug-associated risk. Advise pregnant women and females of reproductive potential of the potential risk to the fetus
- Lactation: There are no data available on the presence of belumosudil or its metabolites in human milk or the effects on the breastfed child, or milk production. Because of the potential for serious adverse reactions from belumosudil in the breastfed child, advise lactating women not to breastfeed during treatment with REZUROCK and for one week after the last dose
- Pediatric Use: The safety and effectiveness of REZUROCK in pediatric patients less than 12 years old have not been established
- Geriatric Use: Of the 186 patients with chronic GVHD in clinical studies of REZUROCK, 26% were 65 years and older. No clinically meaningful differences in safety or effectiveness of REZUROCK were observed in comparison to younger patients
- Renal Impairment: Treatment with REZUROCK has not been studied in patients with pre-existing severe renal impairment. For patients with pre-existing severe renal impairment, consider the risks and potential benefits before initiating treatment with REZUROCK
- Hepatic Impairment: Avoid use in patients with moderate hepatic impairment (Child-Pugh B) or severe hepatic impairment (Child-Pugh C) without liver GVHD. No dose adjustment is recommended for patients with mild hepatic impairment (Child-Pugh A)
Please click here for full Prescribing Information.
INDICATION
REZUROCK® (belumosudil) is indicated for the treatment of adult and pediatric patients 12 years and older with chronic graft-versus-host disease (chronic GVHD) after failure of at least two prior lines of systemic therapy.
IMPORTANT SAFETY INFORMATION
INDICATION
REZUROCK® (belumosudil) is indicated for the treatment of adult and pediatric patients 12 years and older with chronic graft-versus-host disease (chronic GVHD) after failure of at least two prior lines of systemic therapy.
IMPORTANT SAFETY INFORMATION
Warnings and Precautions
- Embryo-Fetal Toxicity: Based on findings in animals and its mechanism of action, REZUROCK can cause fetal harm when administered to a pregnant woman. Advise pregnant women of the potential risk to a fetus. Advise females of reproductive potential and males with female partners of reproductive potential to use effective contraception during treatment with REZUROCK and for one week after the last dose
Adverse Reactions
- The most common (≥ 20%) adverse reactions, including laboratory abnormalities, were infections, asthenia, nausea, diarrhea, dyspnea, cough, edema, hemorrhage, abdominal pain, musculoskeletal pain, headache, phosphate decreased, gamma glutamyl transferase increased, lymphocytes decreased, and hypertension
- Permanent discontinuation of REZUROCK due to adverse reactions occurred in 18% of patients. The adverse reactions which resulted in permanent discontinuation of REZUROCK in > 3% of patients included nausea (4%). Adverse reactions leading to dose interruption occurred in 29% of patients. The adverse reactions leading to dose interruption in ≥ 2% were infections (11%), diarrhea (4%), and asthenia, dyspnea, hemorrhage, hypotension, liver function test abnormal, nausea, pyrexia, edema, and renal failure with (2% each)
- Monitor total bilirubin, aspartate aminotransferase (AST), and alanine aminotransferase (ALT) at least monthly
Drug Interactions
- Proton Pump Inhibitors: Belumosudil exhibits pH-dependent solubility. Concomitant use of REZUROCK with proton pump inhibitors decreases belumosudil exposure, which may reduce the efficacy of REZUROCK. Increase the dosage of REZUROCK when used concomitantly with proton pump inhibitors
- Strong CYP3A Inducers: Belumosudil is a CYP3A substrate. Concomitant use of REZUROCK with strong CYP3A inducers decreases belumosudil exposure which may reduce the efficacy of REZUROCK. Increase the dosage of REZUROCK when used concomitantly with strong CYP3A inducers
- BCRP and OATP1B1 Substrates: Avoid concomitant use with drugs that are BCRP substrates where possible. If used together, monitor patients more frequently for adverse reactions and decrease the BCRP substrates dosage(s) in accordance with the respective Prescribing Information.
Belumosudil is a BCRP inhibitor. Concomitant use of REZUROCK with BCRP substrates increases their plasma concentrations, which may increase the risk of adverse reactions related to these substrates.
Belumosudil is an OATP1B1 inhibitor. Concomitant use of REZUROCK with OATP1B1 substrates may increase their plasma concentrations. Monitor patients more frequently for adverse reactions of these substrates and decrease the OATP1B1 substrates dosage(s) in accordance with the respective Prescribing Information - Certain CYP1A2 and CYP3A Substrates: Avoid concomitant use of REZUROCK with drugs that are sensitive CYP1A2 or CYP3A substrates, for which minimal concentration changes may lead to serious toxicities. If concomitant use cannot be avoided, decrease the CYP1A2 or CYP3A substrate dosage(s) in accordance with the respective Prescribing Information. Belumosudil is a CYP1A2 and CYP3A inhibitor. Concomitant use of REZUROCK with sensitive CYP1A2 substrates (e.g., caffeine) or CYP3A substrates (e.g., midazolam) is predicted to increase CYP1A2 or CYP3A substrate exposure, which may increase the risk of adverse reactions related to these substrates
- Certain UGT1A1 Substrates: Avoid concomitant use of REZUROCK with drugs that are UGT1A1 substrates, for which minimal concentration changes may lead to serious toxicities. If concomitant use cannot be avoided, decrease the UGT1A1 substrates dosage(s) in accordance with the respective Prescribing Information. Belumosudil is a UGT1A1 inhibitor. Concomitant use of REZUROCK with a UGT1A1 substrate decreased plasma concentrations of the glucuronide metabolite of the UGT1A1 substrate. Concomitant use of belumosudil with other UGT1A1 substrates may increase their plasma concentrations, which may increase the risk of adverse reactions related to these substrates
- Certain P-gp Substrates: Avoid concomitant use of REZUROCK with drugs that are P-gp substrates, for which minimal concentration changes may lead to serious toxicities. If concomitant use cannot be avoided, decrease the P-gp substrates dosage(s) in accordance with the respective Prescribing Information. Belumosudil is a P-gp inhibitor. Concomitant use of REZUROCK with P-gp substrates increased their plasma concentrations, which may increase the risk of adverse reactions related to these substrates
Use in Specific Populations
- Pregnancy: There are no available human data on REZUROCK use in pregnant women to evaluate for a drug-associated risk. Advise pregnant women and females of reproductive potential of the potential risk to the fetus
- Lactation: There are no data available on the presence of belumosudil or its metabolites in human milk or the effects on the breastfed child, or milk production. Because of the potential for serious adverse reactions from belumosudil in the breastfed child, advise lactating women not to breastfeed during treatment with REZUROCK and for one week after the last dose
- Pediatric Use: The safety and effectiveness of REZUROCK in pediatric patients less than 12 years old have not been established
- Geriatric Use: Of the 186 patients with chronic GVHD in clinical studies of REZUROCK, 26% were 65 years and older. No clinically meaningful differences in safety or effectiveness of REZUROCK were observed in comparison to younger patients
- Renal Impairment: Treatment with REZUROCK has not been studied in patients with pre-existing severe renal impairment. For patients with pre-existing severe renal impairment, consider the risks and potential benefits before initiating treatment with REZUROCK
- Hepatic Impairment: Avoid use in patients with moderate hepatic impairment (Child-Pugh B) or severe hepatic impairment (Child-Pugh C) without liver GVHD. No dose adjustment is recommended for patients with mild hepatic impairment (Child-Pugh A)
Please click here for full Prescribing Information.
IMPORTANT SAFETY INFORMATION
Warnings and Precautions
- Embryo-Fetal Toxicity: Based on findings in animals and its mechanism of action, REZUROCK can cause fetal harm when administered to a pregnant woman. Advise pregnant women of the potential risk to a fetus. Advise females of reproductive potential and males with female partners of reproductive potential to use effective contraception during treatment with REZUROCK and for one week after the last dose
Adverse Reactions
- The most common (≥ 20%) adverse reactions, including laboratory abnormalities, were infections, asthenia, nausea, diarrhea, dyspnea, cough, edema, hemorrhage, abdominal pain, musculoskeletal pain, headache, phosphate decreased, gamma glutamyl transferase increased, lymphocytes decreased, and hypertension
- Permanent discontinuation of REZUROCK due to adverse reactions occurred in 18% of patients. The adverse reactions which resulted in permanent discontinuation of REZUROCK in > 3% of patients included nausea (4%). Adverse reactions leading to dose interruption occurred in 29% of patients. The adverse reactions leading to dose interruption in ≥ 2% were infections (11%), diarrhea (4%), and asthenia, dyspnea, hemorrhage, hypotension, liver function test abnormal, nausea, pyrexia, edema, and renal failure with (2% each)
- Monitor total bilirubin, aspartate aminotransferase (AST), and alanine aminotransferase (ALT) at least monthly
Drug Interactions
- Proton Pump Inhibitors: Belumosudil exhibits pH-dependent solubility. Concomitant use of REZUROCK with proton pump inhibitors decreases belumosudil exposure, which may reduce the efficacy of REZUROCK. Increase the dosage of REZUROCK when used concomitantly with proton pump inhibitors
- Strong CYP3A Inducers: Belumosudil is a CYP3A substrate. Concomitant use of REZUROCK with strong CYP3A inducers decreases belumosudil exposure which may reduce the efficacy of REZUROCK. Increase the dosage of REZUROCK when used concomitantly with strong CYP3A inducers
- BCRP and OATP1B1 Substrates: Avoid concomitant use with drugs that are BCRP substrates where possible. If used together, monitor patients more frequently for adverse reactions and decrease the BCRP substrates dosage(s) in accordance with the respective Prescribing Information.
Belumosudil is a BCRP inhibitor. Concomitant use of REZUROCK with BCRP substrates increases their plasma concentrations, which may increase the risk of adverse reactions related to these substrates.
Belumosudil is an OATP1B1 inhibitor. Concomitant use of REZUROCK with OATP1B1 substrates may increase their plasma concentrations. Monitor patients more frequently for adverse reactions of these substrates and decrease the OATP1B1 substrates dosage(s) in accordance with the respective Prescribing Information - Certain CYP1A2 and CYP3A Substrates: Avoid concomitant use of REZUROCK with drugs that are sensitive CYP1A2 or CYP3A substrates, for which minimal concentration changes may lead to serious toxicities. If concomitant use cannot be avoided, decrease the CYP1A2 or CYP3A substrate dosage(s) in accordance with the respective Prescribing Information. Belumosudil is a CYP1A2 and CYP3A inhibitor. Concomitant use of REZUROCK with sensitive CYP1A2 substrates (e.g., caffeine) or CYP3A substrates (e.g., midazolam) is predicted to increase CYP1A2 or CYP3A substrate exposure, which may increase the risk of adverse reactions related to these substrates
- Certain UGT1A1 Substrates: Avoid concomitant use of REZUROCK with drugs that are UGT1A1 substrates, for which minimal concentration changes may lead to serious toxicities. If concomitant use cannot be avoided, decrease the UGT1A1 substrates dosage(s) in accordance with the respective Prescribing Information. Belumosudil is a UGT1A1 inhibitor. Concomitant use of REZUROCK with a UGT1A1 substrate decreased plasma concentrations of the glucuronide metabolite of the UGT1A1 substrate. Concomitant use of belumosudil with other UGT1A1 substrates may increase their plasma concentrations, which may increase the risk of adverse reactions related to these substrates
- Certain P-gp Substrates: Avoid concomitant use of REZUROCK with drugs that are P-gp substrates, for which minimal concentration changes may lead to serious toxicities. If concomitant use cannot be avoided, decrease the P-gp substrates dosage(s) in accordance with the respective Prescribing Information. Belumosudil is a P-gp inhibitor. Concomitant use of REZUROCK with P-gp substrates increased their plasma concentrations, which may increase the risk of adverse reactions related to these substrates
Use in Specific Populations
- Pregnancy: There are no available human data on REZUROCK use in pregnant women to evaluate for a drug-associated risk. Advise pregnant women and females of reproductive potential of the potential risk to the fetus
- Lactation: There are no data available on the presence of belumosudil or its metabolites in human milk or the effects on the breastfed child, or milk production. Because of the potential for serious adverse reactions from belumosudil in the breastfed child, advise lactating women not to breastfeed during treatment with REZUROCK and for one week after the last dose
- Pediatric Use: The safety and effectiveness of REZUROCK in pediatric patients less than 12 years old have not been established
- Geriatric Use: Of the 186 patients with chronic GVHD in clinical studies of REZUROCK, 26% were 65 years and older. No clinically meaningful differences in safety or effectiveness of REZUROCK were observed in comparison to younger patients
- Renal Impairment: Treatment with REZUROCK has not been studied in patients with pre-existing severe renal impairment. For patients with pre-existing severe renal impairment, consider the risks and potential benefits before initiating treatment with REZUROCK
- Hepatic Impairment: Avoid use in patients with moderate hepatic impairment (Child-Pugh B) or severe hepatic impairment (Child-Pugh C) without liver GVHD. No dose adjustment is recommended for patients with mild hepatic impairment (Child-Pugh A)
Please click here for full Prescribing Information.
INDICATION
REZUROCK® (belumosudil) is indicated for the treatment of adult and pediatric patients 12 years and older with chronic graft-versus-host disease (chronic GVHD) after failure of at least two prior lines of systemic therapy.
IMPORTANT SAFETY INFORMATION
INDICATION
REZUROCK® (belumosudil) is indicated for the treatment of adult and pediatric patients 12 years and older with chronic graft-versus-host disease (chronic GVHD) after failure of at least two prior lines of systemic therapy.
IMPORTANT SAFETY INFORMATION
Warnings and Precautions
- Embryo-Fetal Toxicity: Based on findings in animals and its mechanism of action, REZUROCK can cause fetal harm when administered to a pregnant woman. Advise pregnant women of the potential risk to a fetus. Advise females of reproductive potential and males with female partners of reproductive potential to use effective contraception during treatment with REZUROCK and for one week after the last dose
Adverse Reactions
- The most common (≥ 20%) adverse reactions, including laboratory abnormalities, were infections, asthenia, nausea, diarrhea, dyspnea, cough, edema, hemorrhage, abdominal pain, musculoskeletal pain, headache, phosphate decreased, gamma glutamyl transferase increased, lymphocytes decreased, and hypertension
- Permanent discontinuation of REZUROCK due to adverse reactions occurred in 18% of patients. The adverse reactions which resulted in permanent discontinuation of REZUROCK in > 3% of patients included nausea (4%). Adverse reactions leading to dose interruption occurred in 29% of patients. The adverse reactions leading to dose interruption in ≥ 2% were infections (11%), diarrhea (4%), and asthenia, dyspnea, hemorrhage, hypotension, liver function test abnormal, nausea, pyrexia, edema, and renal failure with (2% each)
- Monitor total bilirubin, aspartate aminotransferase (AST), and alanine aminotransferase (ALT) at least monthly
Drug Interactions
- Proton Pump Inhibitors: Belumosudil exhibits pH-dependent solubility. Concomitant use of REZUROCK with proton pump inhibitors decreases belumosudil exposure, which may reduce the efficacy of REZUROCK. Increase the dosage of REZUROCK when used concomitantly with proton pump inhibitors
- Strong CYP3A Inducers: Belumosudil is a CYP3A substrate. Concomitant use of REZUROCK with strong CYP3A inducers decreases belumosudil exposure which may reduce the efficacy of REZUROCK. Increase the dosage of REZUROCK when used concomitantly with strong CYP3A inducers
- BCRP and OATP1B1 Substrates: Avoid concomitant use with drugs that are BCRP substrates where possible. If used together, monitor patients more frequently for adverse reactions and decrease the BCRP substrates dosage(s) in accordance with the respective Prescribing Information.
Belumosudil is a BCRP inhibitor. Concomitant use of REZUROCK with BCRP substrates increases their plasma concentrations, which may increase the risk of adverse reactions related to these substrates.
Belumosudil is an OATP1B1 inhibitor. Concomitant use of REZUROCK with OATP1B1 substrates may increase their plasma concentrations. Monitor patients more frequently for adverse reactions of these substrates and decrease the OATP1B1 substrates dosage(s) in accordance with the respective Prescribing Information - Certain CYP1A2 and CYP3A Substrates: Avoid concomitant use of REZUROCK with drugs that are sensitive CYP1A2 or CYP3A substrates, for which minimal concentration changes may lead to serious toxicities. If concomitant use cannot be avoided, decrease the CYP1A2 or CYP3A substrate dosage(s) in accordance with the respective Prescribing Information. Belumosudil is a CYP1A2 and CYP3A inhibitor. Concomitant use of REZUROCK with sensitive CYP1A2 substrates (e.g., caffeine) or CYP3A substrates (e.g., midazolam) is predicted to increase CYP1A2 or CYP3A substrate exposure, which may increase the risk of adverse reactions related to these substrates
- Certain UGT1A1 Substrates: Avoid concomitant use of REZUROCK with drugs that are UGT1A1 substrates, for which minimal concentration changes may lead to serious toxicities. If concomitant use cannot be avoided, decrease the UGT1A1 substrates dosage(s) in accordance with the respective Prescribing Information. Belumosudil is a UGT1A1 inhibitor. Concomitant use of REZUROCK with a UGT1A1 substrate decreased plasma concentrations of the glucuronide metabolite of the UGT1A1 substrate. Concomitant use of belumosudil with other UGT1A1 substrates may increase their plasma concentrations, which may increase the risk of adverse reactions related to these substrates
- Certain P-gp Substrates: Avoid concomitant use of REZUROCK with drugs that are P-gp substrates, for which minimal concentration changes may lead to serious toxicities. If concomitant use cannot be avoided, decrease the P-gp substrates dosage(s) in accordance with the respective Prescribing Information. Belumosudil is a P-gp inhibitor. Concomitant use of REZUROCK with P-gp substrates increased their plasma concentrations, which may increase the risk of adverse reactions related to these substrates
Use in Specific Populations
- Pregnancy: There are no available human data on REZUROCK use in pregnant women to evaluate for a drug-associated risk. Advise pregnant women and females of reproductive potential of the potential risk to the fetus
- Lactation: There are no data available on the presence of belumosudil or its metabolites in human milk or the effects on the breastfed child, or milk production. Because of the potential for serious adverse reactions from belumosudil in the breastfed child, advise lactating women not to breastfeed during treatment with REZUROCK and for one week after the last dose
- Pediatric Use: The safety and effectiveness of REZUROCK in pediatric patients less than 12 years old have not been established
- Geriatric Use: Of the 186 patients with chronic GVHD in clinical studies of REZUROCK, 26% were 65 years and older. No clinically meaningful differences in safety or effectiveness of REZUROCK were observed in comparison to younger patients
- Renal Impairment: Treatment with REZUROCK has not been studied in patients with pre-existing severe renal impairment. For patients with pre-existing severe renal impairment, consider the risks and potential benefits before initiating treatment with REZUROCK
- Hepatic Impairment: Avoid use in patients with moderate hepatic impairment (Child-Pugh B) or severe hepatic impairment (Child-Pugh C) without liver GVHD. No dose adjustment is recommended for patients with mild hepatic impairment (Child-Pugh A)
Please click here for full Prescribing Information.
IMPORTANT SAFETY INFORMATION
Warnings and Precautions
- Embryo-Fetal Toxicity: Based on findings in animals and its mechanism of action, REZUROCK can cause fetal harm when administered to a pregnant woman. Advise pregnant women of the potential risk to a fetus. Advise females of reproductive potential and males with female partners of reproductive potential to use effective contraception during treatment with REZUROCK and for one week after the last dose
Adverse Reactions
- The most common (≥ 20%) adverse reactions, including laboratory abnormalities, were infections, asthenia, nausea, diarrhea, dyspnea, cough, edema, hemorrhage, abdominal pain, musculoskeletal pain, headache, phosphate decreased, gamma glutamyl transferase increased, lymphocytes decreased, and hypertension
- Permanent discontinuation of REZUROCK due to adverse reactions occurred in 18% of patients. The adverse reactions which resulted in permanent discontinuation of REZUROCK in > 3% of patients included nausea (4%). Adverse reactions leading to dose interruption occurred in 29% of patients. The adverse reactions leading to dose interruption in ≥ 2% were infections (11%), diarrhea (4%), and asthenia, dyspnea, hemorrhage, hypotension, liver function test abnormal, nausea, pyrexia, edema, and renal failure with (2% each)
- Monitor total bilirubin, aspartate aminotransferase (AST), and alanine aminotransferase (ALT) at least monthly
Drug Interactions
- Proton Pump Inhibitors: Belumosudil exhibits pH-dependent solubility. Concomitant use of REZUROCK with proton pump inhibitors decreases belumosudil exposure, which may reduce the efficacy of REZUROCK. Increase the dosage of REZUROCK when used concomitantly with proton pump inhibitors
- Strong CYP3A Inducers: Belumosudil is a CYP3A substrate. Concomitant use of REZUROCK with strong CYP3A inducers decreases belumosudil exposure which may reduce the efficacy of REZUROCK. Increase the dosage of REZUROCK when used concomitantly with strong CYP3A inducers
- BCRP and OATP1B1 Substrates: Avoid concomitant use with drugs that are BCRP substrates where possible. If used together, monitor patients more frequently for adverse reactions and decrease the BCRP substrates dosage(s) in accordance with the respective Prescribing Information.
Belumosudil is a BCRP inhibitor. Concomitant use of REZUROCK with BCRP substrates increases their plasma concentrations, which may increase the risk of adverse reactions related to these substrates.
Belumosudil is an OATP1B1 inhibitor. Concomitant use of REZUROCK with OATP1B1 substrates may increase their plasma concentrations. Monitor patients more frequently for adverse reactions of these substrates and decrease the OATP1B1 substrates dosage(s) in accordance with the respective Prescribing Information - Certain CYP1A2 and CYP3A Substrates: Avoid concomitant use of REZUROCK with drugs that are sensitive CYP1A2 or CYP3A substrates, for which minimal concentration changes may lead to serious toxicities. If concomitant use cannot be avoided, decrease the CYP1A2 or CYP3A substrate dosage(s) in accordance with the respective Prescribing Information. Belumosudil is a CYP1A2 and CYP3A inhibitor. Concomitant use of REZUROCK with sensitive CYP1A2 substrates (e.g., caffeine) or CYP3A substrates (e.g., midazolam) is predicted to increase CYP1A2 or CYP3A substrate exposure, which may increase the risk of adverse reactions related to these substrates
- Certain UGT1A1 Substrates: Avoid concomitant use of REZUROCK with drugs that are UGT1A1 substrates, for which minimal concentration changes may lead to serious toxicities. If concomitant use cannot be avoided, decrease the UGT1A1 substrates dosage(s) in accordance with the respective Prescribing Information. Belumosudil is a UGT1A1 inhibitor. Concomitant use of REZUROCK with a UGT1A1 substrate decreased plasma concentrations of the glucuronide metabolite of the UGT1A1 substrate. Concomitant use of belumosudil with other UGT1A1 substrates may increase their plasma concentrations, which may increase the risk of adverse reactions related to these substrates
- Certain P-gp Substrates: Avoid concomitant use of REZUROCK with drugs that are P-gp substrates, for which minimal concentration changes may lead to serious toxicities. If concomitant use cannot be avoided, decrease the P-gp substrates dosage(s) in accordance with the respective Prescribing Information. Belumosudil is a P-gp inhibitor. Concomitant use of REZUROCK with P-gp substrates increased their plasma concentrations, which may increase the risk of adverse reactions related to these substrates
Use in Specific Populations
- Pregnancy: There are no available human data on REZUROCK use in pregnant women to evaluate for a drug-associated risk. Advise pregnant women and females of reproductive potential of the potential risk to the fetus
- Lactation: There are no data available on the presence of belumosudil or its metabolites in human milk or the effects on the breastfed child, or milk production. Because of the potential for serious adverse reactions from belumosudil in the breastfed child, advise lactating women not to breastfeed during treatment with REZUROCK and for one week after the last dose
- Pediatric Use: The safety and effectiveness of REZUROCK in pediatric patients less than 12 years old have not been established
- Geriatric Use: Of the 186 patients with chronic GVHD in clinical studies of REZUROCK, 26% were 65 years and older. No clinically meaningful differences in safety or effectiveness of REZUROCK were observed in comparison to younger patients
- Renal Impairment: Treatment with REZUROCK has not been studied in patients with pre-existing severe renal impairment. For patients with pre-existing severe renal impairment, consider the risks and potential benefits before initiating treatment with REZUROCK
- Hepatic Impairment: Avoid use in patients with moderate hepatic impairment (Child-Pugh B) or severe hepatic impairment (Child-Pugh C) without liver GVHD. No dose adjustment is recommended for patients with mild hepatic impairment (Child-Pugh A)
Please click here for full Prescribing Information.
INDICATION
REZUROCK® (belumosudil) is indicated for the treatment of adult and pediatric patients 12 years and older with chronic graft-versus-host disease (chronic GVHD) after failure of at least two prior lines of systemic therapy.
